10 Causes of Pancreatitis
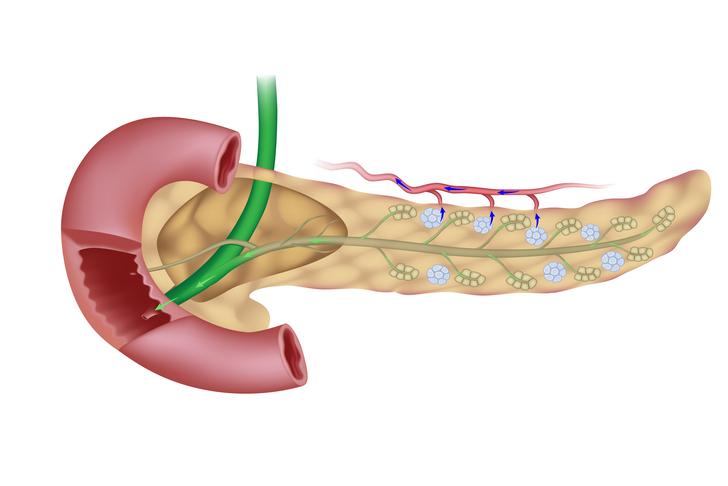
Pancreatitis is a condition characterized by inflammation of the pancreas, an organ that plays a crucial role in digestion and blood sugar regulation. There are two main types of pancreatitis: acute, which occurs suddenly and lasts for days; and chronic, which occurs over many years. Both types can have severe complications if not treated properly. In this article, we will explore 10 common causes of pancreatitis and discuss how to prevent and manage this condition.
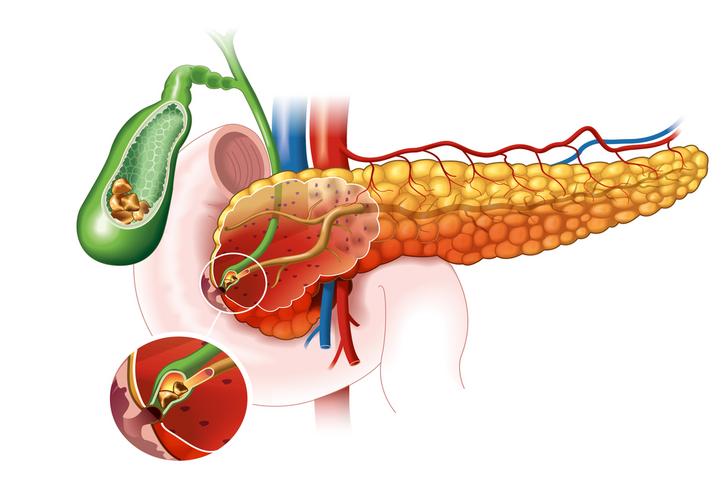
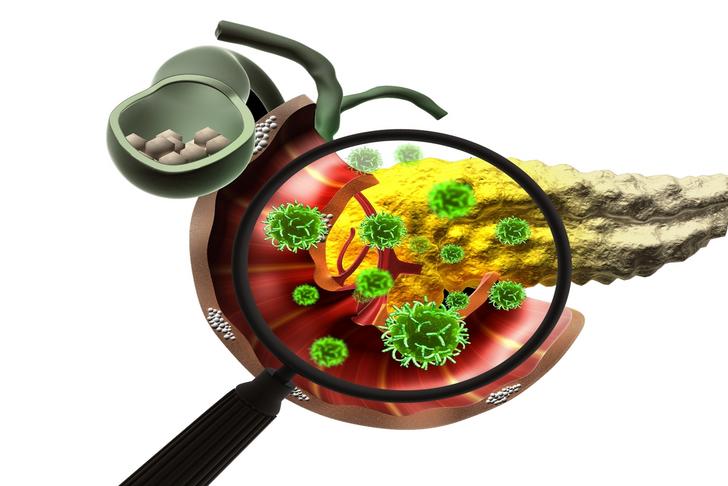
Gallstones
Gallstones are hardened deposits of digestive fluid that can form in the gallbladder. When gallstones block the pancreatic duct, the flow of pancreatic enzymes is disrupted, leading to inflammation and pancreatitis[[1]].
Advertisement
Alcohol Consumption
Excessive alcohol consumption is a leading cause of pancreatitis. Alcohol can cause the pancreas to produce toxic substances that lead to inflammation and damage the pancreatic tissue[[1]].

Advertisement
Smoking
Cigarette smoking is a significant risk factor for both acute and chronic pancreatitis. The chemicals in cigarette smoke can cause inflammation and damage the pancreas, increasing the risk of developing pancreatitis[[2]].

Advertisement
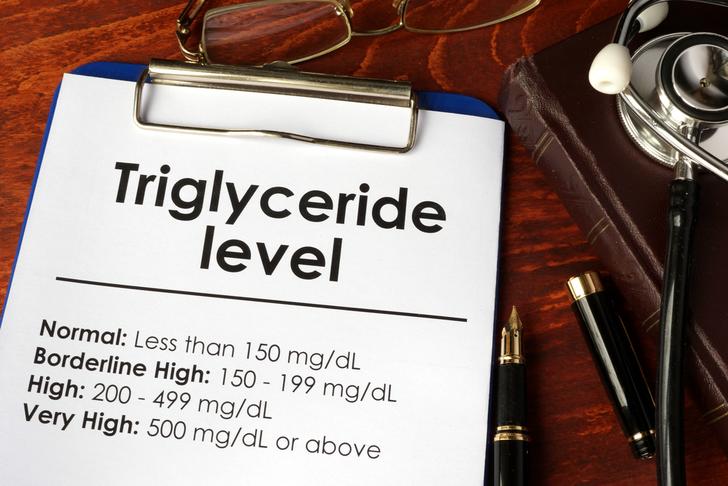
High Triglycerides
Elevated levels of triglycerides, a type of fat found in the blood, can increase the risk of pancreatitis. High triglyceride levels can cause the pancreas to become inflamed and lead to pancreatitis[[1]].
Advertisement
Infections
Certain viral and bacterial infections, such as mumps, hepatitis, and salmonella, can cause inflammation of the pancreas and lead to pancreatitis[[3]].
Advertisement
Autoimmune Diseases
Autoimmune diseases, such as lupus and Sjogren’s syndrome, can cause the immune system to attack the pancreas, leading to inflammation and pancreatitis[[3]].

Advertisement
Medications
Certain medications, including some antibiotics, diuretics, and immunosuppressive drugs, can cause inflammation of the pancreas and increase the risk of pancreatitis[[3]].

Advertisement
Abdominal Injury
Trauma to the abdomen, such as from a car accident or a fall, can cause damage to the pancreas and lead to pancreatitis[[2]].

Advertisement
Pancreatic Cancer
Pancreatic cancer can cause inflammation and blockage of the pancreatic duct, leading to pancreatitis[[2]].

Advertisement
Genetic Factors
Certain genetic mutations can increase the risk of developing pancreatitis. These mutations can cause the pancreas to produce abnormal enzymes or disrupt the normal function of the pancreas[[1]].

Advertisement
Symptoms
Pancreatitis symptoms can vary based on the type, but they may include:
Acute Pancreatitis:
- Upper abdominal pain that may radiate to your back or feel worse after eating.
- Nausea and vomiting
- Fever
- Increased heart rate
Chronic Pancreatitis:
- Upper abdominal pain
- Unintended weight loss
- Oily, smelly stools (steatorrhea)
Advertisement
Treatments
The treatment of pancreatitis depends on the severity and type of the disease. It may include:
Fasting: You may need to stop eating and drinking for a while to allow your pancreas to recover.
Pain management: Pain is a common symptom of pancreatitis. Your doctor might give you medication to help manage the pain.
IV fluids: Dehydration is common with pancreatitis, so liquids are typically provided through a vein.
Nutritional support: Once your pancreas recovers, you may begin a special diet or be given nutritional supplements.
Endoscopic retrograde cholangiopancreatography (ERCP): If gallstones cause your pancreatitis, your doctor may recommend an ERCP to remove them.
Surgery: In severe cases, or if pancreatitis is caused by gallstones, a blocked or narrowed pancreatic duct, or a tumor, surgery may be necessary.
Lifestyle changes: If your pancreatitis is caused by alcohol consumption, you must stop drinking. If high triglyceride levels cause your pancreatitis, you might need to adopt a low-fat diet.
Advertisement
Conclusion
In summing up, pancreatitis is an inflammatory condition of the pancreas that can manifest in both acute and chronic forms. Symptoms often include abdominal pain, nausea, vomiting, and in cases of chronic pancreatitis, unintended weight loss, and oily, foul-smelling stools. The condition can be triggered by various factors such as gallstones, alcohol consumption, and certain medications, making awareness of these causes essential in preventing the onset and managing the progression of this disease.
Treatment strategies for pancreatitis are wide-ranging and depend largely on the specific cause and the severity of the condition. They may involve temporary fasting, pain management, hydration through IV fluids, nutritional support, and surgical interventions. It’s also important to note that specific lifestyle changes may be necessary to effectively manage the condition, mainly related to alcohol consumption or diet.
It is crucial, however, to remember that any treatment approach should be pursued under the guidance of a healthcare provider to ensure it’s safe and suitable for your specific situation. Prompt medical attention is vital if pancreatitis is suspected, as the condition can lead to severe complications if left untreated.
Although pancreatitis is a severe health concern, a thorough understanding of its causes, symptoms, and treatments allows for effective prevention, management, and care. With appropriate healthcare guidance, those dealing with pancreatitis can navigate toward improved health and well-being.
Advertisement